Does an FDA Class 1 Medical Device List Exist?
Understanding where your product falls in FDA classifications can help medical device manufacturers plan for regulatory compliance.
If you can find a substantially equivalent existing device, known as a predicate device, your manufacturing organization will be eligible for a 510(k) application for FDA clearance.
This pathway to regulatory approval is much faster and cheaper than a premarket approval (PMA) approval. 510(k) applications are generally processed by the US FDA within 30-90 days, and human testing is not usually required.
But how do you know if your medical device will be classified as Class I and have a substantial equivalent? We’ll help you understand if a full list exists and the steps you can take to determine your product’s classification. Based on this information, you’ll be in a position to understand your possible pathway to FDA approval.
Does an FDA Class 1 Medical Device List Exist?
Class 1 medical devices are devices with low or moderate risk to patient health and safety. 47% of approved medical devices are Class 1, and 95% of these devices are exempt from the PMA pathway to regulatory approval. Class 1 device manufacturers are required to register their device with the FDA, however. Examples of Class 1 medical devices include bandaids, stethoscopes, and hydrogen peroxide.
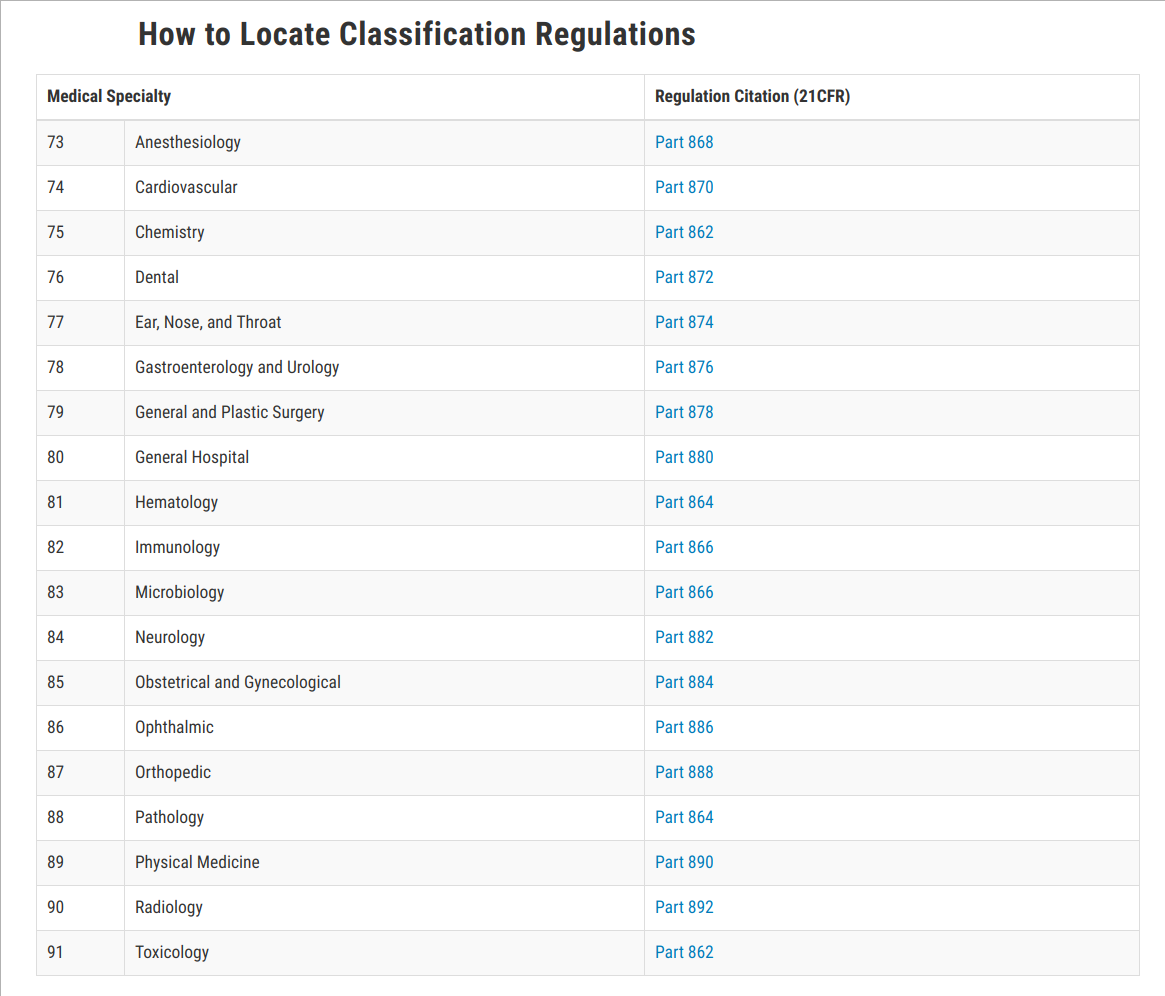
The US FDA is continuously adding medical devices to its searchable databases, which lists approvals, denials, and clearances. Devices are listed among 18 different panels, which group devices according to specializations such as anesthesiology, hematology, and cardiology. The first step towards determining whether your device has a substantial equivalent is to find the right panel classification on the FDA website.
A Constantly Evolving Database, Not a List
The FDA offers an easy-to-use, searchable database for medical device manufacturers to understand approved devices which gained regulatory approval under both the 510(k) and PMA pathway.
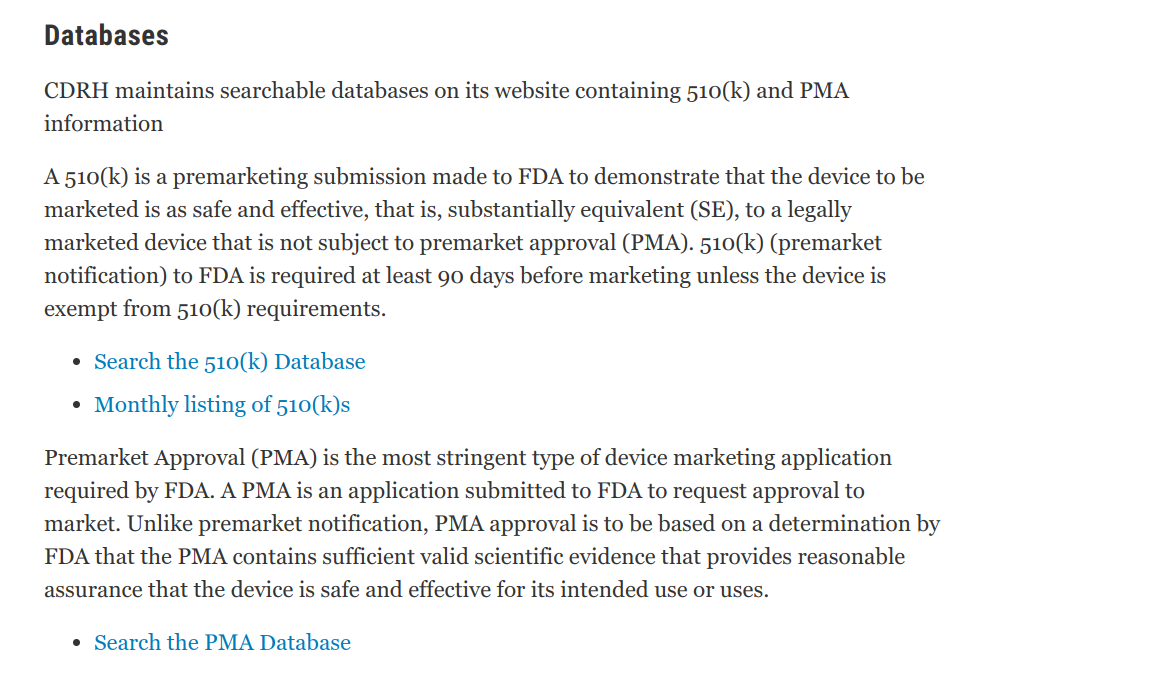
You can use these databases to research substantial equivalence. The FDA maintains these databases instead of a list, since devices are continuously being approved.
RELATED READING: 4 Reasons Overhauling FDA 510(k) is a Great Move
How to Determine Your Product's Category
Understanding the differences in the FDA medical device classes can help you determine whether you’re going to do a 510(k) pathway or PMA. Demonstrating substantial equivalence to products already on the market is generally possible for Class 1 medical devices and many products which fall into Class 2.
- Class 2 devices present moderate risk to the patient or clinical user. 43% of devices regulated by the USA FDA are Class 2. This category includes things like spinal fusion devices or orthopedic implants.
- Class 3 devices are higher-risk and require clinical data to prove safety and efficacy. This category constitutes just 10% of the medical devices the FDA regulates and includes things like cochlear implants and pacemakers.
Risk to the patient is a determining factor in whether your device fits into Class 1, 2, or 3. If your device is very innovative and doesn’t fall into a clear bucket or have a substantial equivalent in the US FDA databases, you’re going to need a premarket approval (PMA) application and clinical data.
When you’re beginning the research process, ask if there is anything on the market in the same space as your device. If your device is completely innovative and designed for an unmet need, there’s a high chance you’ll end up in Class 3. The classification process also considers the device's intended use and any claims about what the device can do for patients. Tweaking label claims can change a device classification in some cases.
510(k) vs. PMA
Manufacturers of medical devices which fall under the PMA pathway are required to demonstrate that the device is safe and effective for the intended use. Manufacturers provide clinical trial data showing device performance on human subjects.
Once devices are approved for market and sale, the FDA can regulate how PMA pathway devices in Class II or III are marketed to ensure manufacturers don’t make any false or misleading claims. Finally, the FDA ensures that marketing communications and labeling for PMA pathway devices include clear information about warnings and contraindications.
One of the key differences between the 510(k) and PMA pathways is that 510(k) devices don’t have to provide clinical data. Instead, according to the FDA, “the manufacturers of 510(k) devices must demonstrate only that these devices have the same intended use and are substantially equivalent to these similar...devices.”
The 510(k) pathway for approval is much faster than a PMA. 510(k) devices are generally approved within 30-90 days, while PMA devices which meet the FDA’s threshold for application quality are subject to a 180-day review period.
In addition, the 510(k) pathway is much cheaper. The fee for a 510(k) application in 2019 is $10,953 and $2,738 for small businesses. A PMA costs $322,147 or $80,537 for small businesses. Your organization can pay the reduced rate for either pathway if your gross receipts and sales for the prior year are less than $100 million, and you submit a formal FDA small business certification request.
Developing a Quality-Driven Company Focus
Understanding the probable classification of your medical device prior to regulatory approval is important for device manufacturers. Since the PMA pathway to regulatory approval is much more resource-intensive than the 510(k) alternative, it’s beneficial to know what to expect in advance.
You can expect streamlined compliance requirements if your device falls into Class I or Class 2 with a substantial equivalent. Getting ahead of compliance can help your organization create a strong baseline, allocate resources, and avoid regulatory snags.
Regardless of whether your medical device is a Class 1, 2, or 3, creating a quality-driven company focus can be a competitive advantage. Instead of viewing compliance as a checklist and meeting minimum thresholds for FDA approval, a quality-driven culture focuses on continuous improvement to create the best possible devices for patients.
